The Omicron Best-Case and Worst-Case Scenarios
What the coming weeks could bring if we’re lucky. Or not so lucky.
Governments, businesses, and consumers are tipping back into heightened emergency mode as the news sinks in about the Omicron wave of COVID-19 and its rapid spread. Although it is still too early to say anything definitive, there is reason to hope that Omicron may prove less dangerous than previous variants—and may even, if we’re very lucky, bring the world closer to the end of the pandemic. Omicron first appeared in late November like a nightmare apparition exploding from a coffin, spreading twice as fast as the highly infectious Delta variant. From the available evidence, Omicron seems to be much more capable of punching through two vaccine doses: More than a hundred people caught it at a single Christmas party in Norway, and every single one of them was vaccinated. Omicron struck with full force in South Africa after the Delta surge there had already subsided, but in the United States and Europe it’s hitting while infections and hospitalizations from Delta are still quite high. European countries from Denmark to Slovakia have heavier caseloads than ever. Several states in the Northeastern United States—Maine, Vermont, New Hampshire—have seen new records for COVID hospitalizations in the last few days and weeks, as has Michigan. Other states are nearing their previous hospitalization peaks. Mind you, all of this is with over 60 percent of the U.S. population having received two or more vaccine doses and with those Northeastern states above the national average. So much for the bad news. Before turning to the potential silver linings, let’s double-underline a few caveats.
Omicron was originally detected in samples collected just five weeks ago, so we are still in the early days and the epidemiological data is limited.
No major studies with large sample sizes have been published by scientific outlets yet.
That leaves us right now extrapolating from preliminary studies, which may later prove flawed, and from publicly available data, which raises its own difficulties, as Maimuna Majumder noted last week:
I think we need to be really careful about making generalizations regarding the observed transmissibility & virulence of omicron across countries. What's happening in Country X may not translate to Country Y because of differences in epidemic dynamics, demographics, & policies.
— Dr. Maimuna Majumder (@maiamajumder) December 17, 2021
While this thread is about generalizability of observations across countries, much of my team's work is about heterogeneity at the sub-national level. No country is a monolith, & this is uniquely true IMO for settings like the US. Let's take care before generalizing here as well.
— Dr. Maimuna Majumder (@maiamajumder) December 17, 2021
With those caveats in mind, let’s tick through what we think we know about Omicron and how firmly we think we know it.
Last week saw the release of a preliminary finding that may explain why Omicron spreads differently from previous variants. A Hong Kong University study with an unknown sample size of infected human tissues, now under peer review for publication, found that Omicron multiplies 10 times slower in the lungs—but 70 times faster in the airways—than previous variants. This pathology could explain why Omicron generally seems to cause less severe symptoms and why it is more transmissible. What does this apparently milder but more transmissible variant look like in a clinical setting? Here is how Discovery Health, South Africa’s largest private health insurance company, last week summarized the findings of more than 200,000 COVID tests during the first three weeks of that country’s Omicron wave: “The risk of hospital admission among adults diagnosed with COVID-19 is 29% lower for the Omicron variant infection compared to infections involving the D614G mutation in South Africa’s first wave in mid-2020, after adjusting for vaccination status.” To temper this good-sounding evidence, the company’s CEO notes that the lower hospitalization percentage could partly be the result of the high presence of COVID “antibodies in the general South African population, especially following an extensive Delta wave of infections.” Another suggestive indicator comes from Netcare, South Africa’s largest network of private health care providers. Its CEO, who works as a physician in Guateng Province (Pretoria), an Omicron hotspot, estimated on December 8 that only about 10 percent of Netcare’s COVID patients during the present fourth wave require some form of oxygen therapy—as compared to nearly 100 percent during the first three waves. Doctors at another major hospital complex in Pretoria also reported in early December that a surprisingly low number of COVID patients required supplemental oxygen and that the majority are now “incidental COVID admissions”—that is, patients who have COVID but who were admitted for some non-COVID reason:
This is a picture that has not been seen in previous waves. In the beginning of all three previous waves and throughout the course of these waves, there has always only been a sprinkling of patients on room air in the COVID ward and these patients have usually been in the recovery phase. . . . The COVID ward was recognizable by the majority of patients being on some form of oxygen supplementation with the incessant sound of high flow nasal oxygen machines, or beeping ventilator alarms.
Patients in South Africa are reportedly also spending less time in the hospital. If Omicron truly does trend toward less hospitalization and, in cases where the patient does require a hospital, shorter and less catastrophic stays, then perhaps the load on healthcare systems we’re expecting from the Omicron surge will be less, on a per-diagnosis basis, than we saw from previous waves. We’ll find out soon enough because Omicron is bearing down on us much faster than previous waves. In the United Kingdom—where the COVID team at Imperial College London has not found evidence that Omicron is less severe than Delta, as the evidence from South Africa suggests—cases of the new variant doubled roughly every 2.5 days:
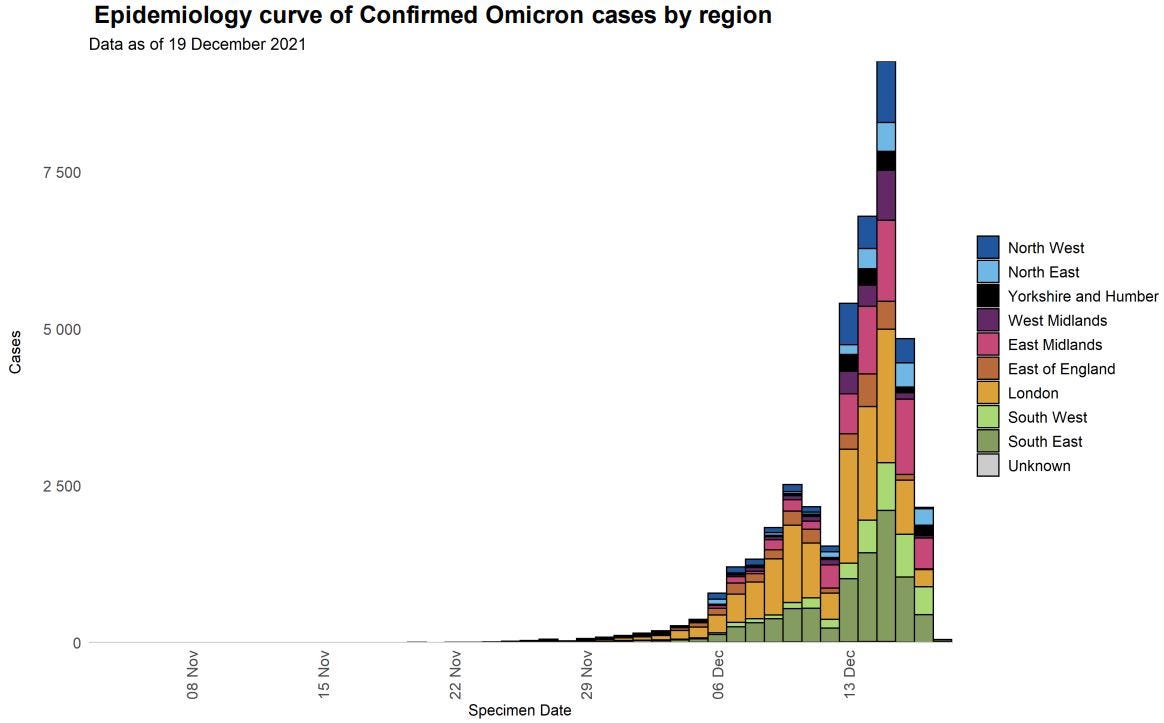
(U.K. Health Security Agency) That high rate shouldn’t last, of course—eventually Omicron won’t find new hosts as easily—and it won’t be the same everywhere, but one implication is clear: A huge percentage of people will be falling ill at the same time, and not just where you live but all over the world. We could have big problems if even a tiny percentage need to be hospitalized.
Let’s take a step back now and, with the help of public health experts, look at Omicron’s part in the overall COVID picture. When the pandemic first hit, a small percentage of a large number of people got severely ill. Although further data may change the outlook, it appears that in the Omicron wave we may see an even smaller percentage of an even larger number of people get severely ill. How does that play out in the real world? We don’t know. And it won’t play out the same everywhere because conditions are different everywhere. Just as a for-instance: The median age in South Africa is 28.0 years, while in the United States it’s 38.5 and in Germany it’s 47.8. To date, previous COVID variants have tended to hit older populations harder than younger populations. Then there’s the question of vaccine coverage: In the United States, it’s roughly double what it is in South Africa, and it’s even higher in most of Europe. And we still don’t know how well vaccines work against Omicron. Preliminary data from South Africa and the United Kingdom suggests that two doses of Pfizer are only around 30-40 percent effective, but booster shots raise the effectiveness to upwards of 70 percent. All of these conditions—average age, share of previously infected, share vaccinated, share boosted, access to medical care—will mean that every country can expect its own experience with Omicron. It could easily overwhelm hospitals all over again, at least in some places. It’s not inconceivable that tens of millions of people—perhaps even hundreds of millions all over the world—will soon be calling in sick during the same week. Maybe this is no big deal if all you do is spend a few days on the couch popping Tylenol and binge-watching Netflix. But there is a global supply chain, and there are critical industries. The height of the Omicron surge would be a bad time to get, say, a catastrophic weather event, like the one that disrupted natural gas supplies in Texas last year. Which brings us to one of the most important unknowns about Omicron: To what extent will an Omicron infection confer immunity against other strains? Here is the best-case scenario—keeping in mind that we don’t have nearly enough data yet: Omicron infections tend to be milder than Delta infections. The case fatality rate and infection fatality rate for Omicron are significantly lower than for Delta. Omicron winds up conferring some protection against Delta and other strains of COVID. And Omicron’s heightened infectiousness allows it to outcompete Delta and replace Delta as the dominant strain of COVID. In this scenario—in the long run—Omicron could wind up saving lives on balance by replacing Delta with a less deadly but more infectious version of COVID. A significant percentage of those who wouldn’t have survived Delta will survive Omicron and then have some protection against Delta and future variants. It is even possible to imagine a scenario in which Omicron could be the means by which COVID moves from pandemic to endemic—by quickly ensuring that almost everybody in the world is at least partially “immunized.” The enormous uncertainties surrounding immunity and reinfection make it impossible to know how likely this optimistic scenario is. But a few scientists and public health experts have been willing to discuss that possibility, with the requisite hedging and caveats. Here’s Monica Gandhi of UCSF in New York magazine: “Omicron could still be really bad—we don’t know yet—but in the best case scenario it would hasten the time when we’re all immune and the pandemic essentially comes to an end.” And the new German health minister, Karl Lauterbach, speculated a few weeks ago that Omicron may be a “Christmas gift” if it makes the pandemic end sooner. Something along those lines is what brought the 1918 “Spanish flu” to an end. After killing between 50 million and 100 million people worldwide, it finally stopped after the virus was forced by widespread immunity to mutate into a less lethal version of itself. And of course, it’s possible to imagine a much worse scenario: Omicron turns out to be only marginally less deadly, once you adjust for external factors, and is so distinct from Delta that rather than displacing it, the two strains live side by side. This would be very not good. After the last two years, some of us have been conditioned to expect the worst. But contrary to recent history, the worst doesn’t always show up. And after the run the world has had over the last two years, it sure seems like we should be due some good luck.